Your blood goes from your heart to your lungs through your pulmonary artery.
In the lungs, the blood is supplied with oxygen, and then it goes back to the heart, which pumps the oxygen-rich blood to the rest of your body.
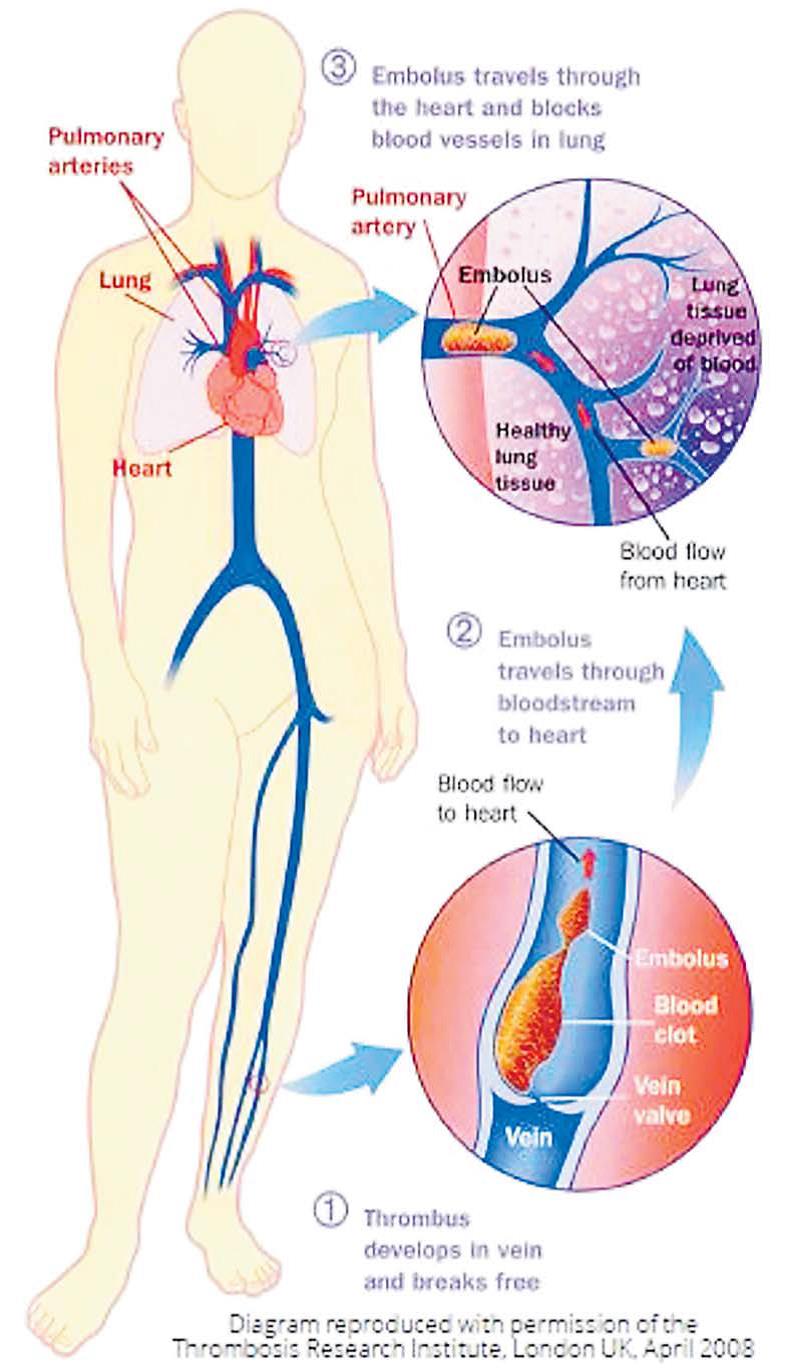
When a blood clot gets caught in one of the arteries that go from the heart to the lungs, it’s called a pulmonary embolism (PE).
The clot blocks the normal flow of blood.
This blockage can cause serious problems, like damage to your lungs and low oxygen levels in your blood.
The lack of oxygen can harm other organs in your body, too. If the clot is big or the artery is clogged by many smaller clots, a pulmonary embolism can be deadly.
Pulmonary embolisms usually travel to the lungs from a deep vein in the legs.
This is called deep vein thrombosis (DVT).
These clots develop when the blood can’t flow freely through the legs because your body is still for a long time, say during a long flight or drive.
It might also happen if you’re on bed rest after surgery or illness.
What else could raise my chances of having a PE?
The risk factors are the same as those for DVT.
These is called the Virchow’s triad.
They are: Not moving for a long time or having changes in normal blood flow.
This often happens if you’ve been in the hospital or on bed rest for a long period of time.
It could also happen during a long flight or vehicle ride.
Blood that’s more likely to clot.
Is called hypercoagulability.
It could be caused by medications, like birth control pills.
Smoking, cancer, recent surgery, or pregnancy can also put you at risk.
Damage to a blood vessel wall.
Injury to your lower leg can lead to this.
In rare cases, an artery in the lung can be blocked by something other than a clot, like an air bubble or part of a tumor.
If you break a big bone, fat from the bone marrow can sometimes come through the blood and cause blockage.
How can I prevent a pulmonary embolism?
The best way to prevent a PE is to try to stop blood clots from forming deep in your veins.
This can be challenging if you’ve been on bed rest after a surgery or illness, or if you just took a long flight.
If you’re at risk, here are a few things that may help lower your chances of getting these dangerous blood clots:
Blood thinners
The use of anticoagulants.
They keep your blood from forming clots.
Your doctor might also recommend blood thinners if you’ve been hospitalised after a stroke or heart attack, or if you have complications from cancer.
Compression stockings
These are long socks that squeeze your legs.
The extra pressure helps blood move through your veins and leg muscles.
It is recommended that you wear them for a while after surgery.
Exercise
Get out of bed and walk when you’re getting over a long stay in the hospital or an illness that’s kept you in bed for too long.
It’ll keep the blood in your legs flowing so it doesn’t have a chance to pool.
Stretching during trips
If you’re on a long flight, try to walk around every few hours.
If you can’t stand up, flex your ankles by pulling your toes toward you.
Here’s another stretch you can try to do while seated:
Pull your leg up toward your chest with one hand;
Hold the bottom of that leg with the other hand;
Keep this pose for 15 seconds, and then try it with the other leg; and
Do this up to 10 times per hour.
If you’re driving a long distance, stop every hour and stretch your legs.
Also, be sure to drink extra fluids to help you stay hydrated.
Lifestyle changes
Other steps you can take include:
Maintain a healthy weight;
If you plan to take hormones, like birth control or replacement therapy, talk to your doctor about your risk for blood clots;
If you have other health issues, like diabetes or heart failure, take your meds, watch what you eat, and talk to your doctor about any changes;
Also talk to your doctor if you have a history of kidney disease or certain autoimmune diseases, or a family history of blood clots; and
If you smoke, quit.
In life-threatening cases of pulmonary embolism, your doctor may decide to give you drugs called thrombolytics to break up the clot.
It may even need to be taken out or broken up with surgery, though this is rare.
When an artery in your lung gets blocked by a blood clot, you have a pulmonary embolism (PE).
Symptoms can vary.
What you experience will likely depend on the size of the clot and how much of your lung it affects.
‘If you have lung or heart disease, that can play a role, too.
PE is a medical emergency
Symptoms of PE tend to come on suddenly.
– Shortness of breath;
– Chest pain;
– Cough (it may be bloody, and there might be blood in the gunk you cough up);
– Sudden pain in your back;
– Much more sweating than usual;
– A lightheaded feeling, or passing out; and
– Blue lips or nails.
Warning signs of deep vein thrombosis
When a clot forms in a deep vein in your legs, it’s called deep vein thrombosis (DVT).
If it breaks off and travels to your lung, it becomes a pulmonary embolism.
See your doctor right away if you have any of the symptoms of DVT.
If it’s found early, doctors can stop it from becoming a pulmonary embolism.
Signs of DVT include:
Swelling of a leg or arm;
Leg pain or tenderness when you’re standing or walking;
A swollen leg or arm that feels warmer than normal;
Red or discoloured skin in the affected arm or leg; and
Veins in your arm or leg that are larger than normal.
If you think you have a pulmonary embolism (PE), you should get medical help right away.
Your doctor will likely start with a physical exam.
They’ll look closely at your legs to see if they’re swollen, tender, discoloured, or warm.
These are signs that you may have a clot deep in one of your veins.
Next, the doctor may order a number of tests, like a chest X-ray or ultrasound.
You might also have blood tests.
These can measure the amount of oxygen and carbon dioxide in your blood.
They can also help detect a substance called D dimer.
This is a small protein fragment that’s present in the blood after a clot is broken down by the body.
Other tests your doctor might order include:
Computed tomographic pulmonary angiography (CTPA).
This is a special type of X-ray test.
It’s also the main one used to see if you have a PE.
Some dye (contrast) is injected into the veins.
They’ll be able to see the blood vessels in your lungs on the X-ray.
Ventilation/perfusion (V/Q) scan.
This test is used if the CTPA isn’t available, or isn’t a good match for you.
It uses a radioactive material to show which parts of your lungs are getting air flow (ventilation) and blood flow (perfusion).
If there’s low blood flow to a certain area, but the air fl ow is normal, a clot may be present.
A pulmonary embolism (PE) is a blood clot in the lung that has dislodged from a vein and travels through the bloodstream.
It’s serious and can be life-threatening.
But the good news is that if it’s caught early, doctors can treat it.
Here’s a look at some of the most common ways in which it is tackled.
Blood thinners
Also called “anticoagulants,” these are the most common treatment for a blood clot in the lung.
They serve two key roles:
First, they keep the clot from getting any bigger.
Second, they keep new clots from forming.
They don’t dissolve blood clots.
Your body normally does that on its own over time.
The most commonly prescribed blood thinners are warfarin and heparin.
Treatment can begin while you’re in the hospital or even in the emergency area and you can be discharged the same day.
How long you’ll stay and be treated depends on your condition.
Low-molecular-weight heparins are also widely used.
These can be self-injected at home.
They include:
– Dalteparin (Fragmin);
– Enoxaparin (Lovenox); and
– Tinzaparin (Innohep).
In life-threatening situations, doctors might use what are called thrombolytic drugs.
These quickly break up clots that cause severe symptoms.
But they can lead to sudden bleeding and are only used after careful consideration.
Embolectomy
In carefully selected cases, this is another emergency treatment your doctor might use.
They’ll insert a thin, flexible tube into a vein in your thigh or arm.
They’ll continue on to your lung, where they’ll remove the clot or use medicine to dissolve it.
As the saying goes prevention is better than cure, so let’s prevent:
Exercise regularly.
If you can’t walk around due to bed rest, recovery from surgery or extended travel, move your arms, legs and feet for a few minutes each hour.
If you know you will need to sit or stand for long periods, wear compression stockings to encourage blood flow.
Drink plenty of fluids, like water and juice, but avoid excess alcohol and caffeine.
If you need to be stationary for long periods of time, move around for a few minutes each hour: move your feet and legs, bend your knees, and stand on tip-toe.
– Do not smoke;
– Avoid crossing your legs;
– Do not wear tight-fitting clothing;
– Lose weight if you are overweight; and
– Elevate your feet for 30 minutes twice a day.
Talk to your doctor about reducing your risk factors, especially if you or any of your family members have experienced a blood clot.
- Dr. Romika Singh is a general practitioner at Oceania Hospitals Pte Ltd. The views expressed are her own and do not necessarily reflect the views of this
newspaper.